Advanced Pain Management in Root Canal Therapy - Practical Solutions
Pain during and after root canal treatment is one of the biggest challenges clinicians face. Despite improvements in techniques, up to 40% of patients report some degree of postoperative pain1.
Managing this pain effectively is key to improving patient comfort, satisfaction, and clinical outcomes.
Here is what every dental practitioner should know about advanced pain management in endodontics.
Why Does Pain Occur in Root Canal Therapy?
Pain can arise from multiple factors:
- Inflammation of pulp and periapical tissues
- Mechanical irritation during instrumentation
- Chemical irritation from irrigants or medicaments
- Incomplete anesthesia or nerve sensitization
Having a clear idea about the causes can help tailor pain management strategies.
Pain Management - What Should You Know?
Understanding the different stages of anesthesia and key pain management strategies is essential for effective root canal treatment.
Preemptive Analgesia
Preemptive analgesia refers to the administration of analgesics before a painful stimulus, here for a root canal procedure, with the goal of:
- Reducing central sensitization of the nervous system
- Minimizing postoperative pain intensity
- Enhancing patient comfort immediately after treatment2
Recommendations -
NSAIDs, especially ibuprofen 400-600 mg, taken 1 hour prior, are most effective.
- Combining acetaminophen with ibuprofen shows superior pain control3.
- Assess preoperative pain levels with the Visual Analog Scale (VAS) for better planning.
Optimizing Anesthesia
Achieving profound anesthesia can be difficult in cases of irreversible pulpitis or inflamed tissues.
Recommendations:
- Use supplemental injections like intraligamentary or intraosseous anesthesia to improve success when standard nerve blocks fail4.
- Prefer 4% articaine with epinephrine for better nerve penetration and faster onset compared to 2% lidocaine5.
- Use buffered anesthetics to reduce injection pain and speed onset6.
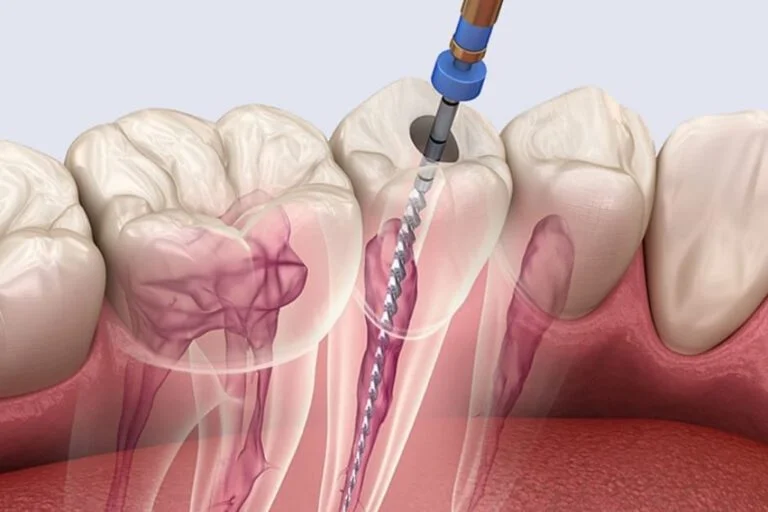
Minimize Procedural Trauma
- Use nickel-titanium rotary files with controlled torque to reduce mechanical irritation and inflammation7.
- Avoid over-instrumentation and carefully maintain apical patency to minimize postoperative pain.
Adjunctive Strategies to Reduce Pain
Here are a few additional methods that can help regulate pain -
- Intracanal corticosteroids reduce periapical inflammation and postoperative pain.
- Cryotherapy with cold saline irrigation lowers tissue temperature, reducing inflammatory mediators8.
- Low-Level Laser Therapy (LLLT) helps modulate inflammation and promotes healing9.
Postoperative Pain Control Protocol
- NSAIDs remain first-line analgesics for managing postoperative pain.
- Combining acetaminophen and NSAIDs maximizes analgesic effects and reduces side effects10.
- Educate patients about expected pain and provide clear instructions to improve compliance.
Managing Pain in Complex Cases and Retreatment
- Retreatment cases often have persistent infection and anatomical challenges that increase pain risk.
- Use multimodal analgesia (NSAIDs + corticosteroids + adjuncts) for better control11.
- Refer for surgical intervention if pain persists despite nonsurgical efforts.
Key Takeaways for Clinicians
- Preemptive analgesia reduces pain intensity.
- Supplemental anesthesia techniques increase success in difficult cases.
- Minimally traumatic instrumentation lowers postoperative inflammation.
- Adjunct therapies like corticosteroids and cryotherapy enhance pain control.
- Clear patient communication improves pain management outcomes.
Final Thoughts
Managing pain in root canal therapy is more than just medication; it involves using the right techniques and tools to make the entire experience easier for your patients.
Combining effective anaesthesia, gentle procedures, and helpful extras like corticosteroids or cryotherapy can provide extra comfort.
And don’t forget, clear communication about what to expect goes a long way in helping patients feel comfortable and confident.
Nailing these key steps can turn a tough treatment into a smooth, pain-free experience.
References
- Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod. 2011 Apr;37(4):429-38.
- Moore PA, Hersh EV. Combining ibuprofen and acetaminophen for acute pain management after third-molar extractions: translating clinical research to dental practice. J Am Dent Assoc. 2013;144(8):898–908.
- Cooper SA, Patel N, et al. Synergistic effect of acetaminophen and ibuprofen on pain: a clinical trial. Pain. 2017;158(5):1001-1008.
- Aggarwal V, Singla M, Miglani S, Kohli S, Sharma V, Bhasin SS. Does the volume of supplemental intraligamentary injections affect the anaesthetic success rate after a failed primary inferior alveolar nerve block? A randomized-double blind clinical trial. Int Endod J. 2018 Jan;51(1):5-11.
- Syed GA, Mulay SA. Comparative evaluation of anesthetic efficacy of 4% articaine and 2% lidocaine for buccal infiltration in adult patients with irreversible pulpitis of maxillary first molar: a prospective randomized study. Contemp Clin Dent. 2022 Jan-Mar;13(1):61-68.
- Malamed SF. Handbook of Local Anesthesia. 7th ed. Elsevier; 2017.
- Plotino G, Grande NM, Cotti E, Testarelli L, Gambarini G. Blue treatment enhances cyclic fatigue resistance of vortex nickel-titanium rotary files. J Endod. 2014 Sep;40(9):1451–3.
- Hespanhol FG, Guimarães LS, Antunes LAA, Antunes LS. Effect of intracanal cryotherapy on postoperative pain after endodontic treatment: systematic review with meta-analysis. Restor Dent Endod. 2022 Jul 4;47(3):e30.
- Guerreiro MYR, Monteiro LPB, de Castro RF, Magno MB, Maia LC, Brandão JMS. Effect of low-level laser therapy on postoperative endodontic pain: An updated systematic review. Complement Ther Med. 2021 Mar;57:102638.
- Derry CJ, Derry S, Moore RA. Single dose oral ibuprofen plus paracetamol (acetaminophen) for acute postoperative pain. Cochrane Database Syst Rev. 2013 Jun 24;2013(6):CD010210.
- Iranmanesh F, Parirokh M, Haghdoost AA, Abbott PV. Effect of corticosteroids on pain relief following root canal treatment: a systematic review. Iran Endod J. 2017;12(2):123–130.
Related Content
Tackling Calcified and Curved Canals
Let’s be real, tackling a stubborn calcified canal is not only a nuisance, it is a true litmus test for endodontic skills. To make it easier to handle the situation for the next case, here are a few subtle “tricks of the trade” that can help conquer these cases confidently and consistently. Why Calcified & Curved Canals Wreck More Cases Than You Think? Here is what one should know: up to 60% of root canal failures involve missed or inadequately treated canals, many of which are calcified or severely curved. These canals pose a triple threat: Hard to detect: Pulp chambers disappear like mirages on X-rays Hard to negotiate: Files bend, bind, or break mid-operation Hard to disinfect: Bacterial biofilms thrive in untouched canal recesses. If the clinician does not tackle these challenges head-on, they might be looking at a compromised prognosis with frustrated patients. 7 Clinical Hacks to Crack Calcified Canals Without Guesswork 1. Champagne Bubble Test The "Champagne Bubble Test" involves applying sodium hypochlorite (NaOCl) to the pulp chamber and observing for effervescence.1 Positive effervescence indicates the presence of organic tissue in hidden canals. This test is non-invasive and requires no additional equipment, making it a practical choice in routine endodontic procedures. 2. C-Pilot Files Combined with EDTA and Microultrasound Navigating calcified canals can be challenging. The combination of EDTA, C-Pilot files, and microultrasound can help by improving canal negotiation.2 The use of EDTA helps in chelating calcium ions, softening the calcified tissue, and, in addition, microultrasound aids in precise canal negotiation. 3. Reciprocating Motion in Curved Canals Reciprocating motion with clockwise 140 degrees and counterclockwise 45 degrees has been proposed to reduce the risk of file separation in curved canals.3 Utilizing reciprocating systems like WaveOne Gold can enhance safety and efficiency in curved canal preparation. 4. Pre-Bending Files for Canal Negotiation Pre-bending files is an effective yet overlooked trick in navigating calcified or curved canals. Endodontists with years of experience recommend this for the practicality in negotiating challenging canals. 5. Tapered Access Preparation for Improved Canal Entry Creating a tapered access cavity facilitates straight-line access to the canal system. Wider coronal prep is standard in endodontic access preparation, which helps reduce the file stress and improves canal negotiation. Focusing on the glide path improves file centring and minimises perforation risk.4 6. Use Warm NaOCl with Passive Ultrasonic Irrigation (PUI) Heat sodium hypochlorite to 40°C and activate with ultrasonic agitation (e.g. IrriSafe). Studies show that this method removed 65% more biofilm than syringe irrigation.5 7. Heat-Treated NiTi Files Traditional stainless steel files snap under stress in curved canals. Switch to heat-treated NiTi files like HyFlex EDM or ProTaper Gold that ‘remember’ their shape but stay flexible enough to navigate bends gracefully. Use a gentle, pecking motion with minimal force without rushing the glide path. Mastery and Mishap Extreme curvatures (>25°) demand respect and finesse. Here is a summary of how to stay in control: Always create a glide path with small hand files to reduce torsional stress on rotary instruments. Use a ‘crown-down’ approach, enlarging coronal thirds first to improve straight-line access. Opt for controlled memory NiTi files that adapt to canal curvature without forcing the shape. Avoid forcing files when resistance is felt. Retreat and reassess with irrigants or ultrasonic agitation. Be mindful of your working length at all times. Over-instrumentation risks ledging and perforation. Final Thoughts Managing calcified and curved canals is about strategy, not struggle. With the right tools, protocols, and insight, you can reduce failures and increase case predictability, all while preserving your confidence (and your rotary files). References Mirza AJ, Faruqi FA, Moosa R. Champagne bubble test: An authentic method to find hard-to-find canals during root canal therapy. Acta Sci Dent Sci. 2021;5(10):68-71. Chu T, Ni X, Zhu Y. EDTA combined with C-Pilot files and microultrasound for root canal calcification: dredging effect and safety analysis. Comput Math Methods Med. 2022;2022:1911448. You SY, Kim HC, Bae KS, Baek SH, Kum KY, Lee WC. Shaping ability of reciprocating motion in curved root canals: a comparative study with micro-computed tomography. J Endod. 2011 Sep;37(9):1296-300. Lup VM, Malvicini G, Gaeta C, Grandini S, Ciavoi G. Glide path in endodontics: A literature review of current knowledge. Dent J (Basel). 2024 Aug 14;12(8):257. Joy J, Mathias J, Sagir VM, Babu BP, Chirayath KJ, Hameed H. Bacterial biofilm removal using static and passive ultrasonic irrigation. J Int Oral Health. 2015 Jul;7(7):42–7.
Article
Retreatment or Surgery? Your Step-by-Step Decision Tree When a Root Canal Fails
Even with meticulous technique, root canal treatments may occasionally fail. Despite our best efforts, failure occurs, and the rates range between 10% to 20%. When they do, clinicians must answer a critical question: Do you retreat the canal or opt for surgical intervention? Such decisions are rarely straightforward, but a clear framework can guide clinicians toward the most patient-centered solution. Why Do Root Canals Fail? Understanding the reason for failure is step one. The top causes of root canal failure include1: Missed canals (especially MB2 in maxillary molars) Inadequate cleaning and shaping Persistent periapical infection Leakage from coronal restorations Instrument separation or ledges Research highlighted that missed anatomy and persistent intraradicular infection were the most common causes of persistent apical periodontitis after RCT2. When Is Retreatment the Right Choice? Retreatment is a non-surgical endodontic retreatment that involves removing the old filling, disinfecting the canal, and refilling. Retreatment is Recommended When: There is access to the canal system The cause of failure is missed anatomy or inadequate previous treatment The restoration is either temporary or easily replaced The tooth is structurally sound and restorable Retreatment success rates range from 75% to 88%, with the use of modern techniques such as CBCT, magnification, and bioceramic sealers3. Retreatment preserves more of the natural tooth and is often preferred when feasible. When Does Surgery Make More Sense? Apicoectomy is the surgical option that involves root-end resection, curettage, and retrograde filling, with the help of magnifying tools. Consider Surgery When: The canal is blocked by posts or ledges that cannot be bypassed Retreatment has failed or is not technically possible There is a persistent periapical lesion or cyst that does not resolve A perforation or complex resorption is present Evidence-Based Stats: Recent studies show that apicoectomy, especially when performed using modern microsurgical techniques delivers excellent short-term outcomes. Healing rates in the first 2 to 4 years have been reported as high as 85% to 95%4. However, long-term success tends to taper. Studies following up over 5 to 10 years report success rates in the range of 60% to 80%, depending on the clinical situation5. What do we learn from this? Apicoectomy can be highly successful, especially in the short term, but it is essential to set realistic expectations and choose cases wisely. Decision-Making Guide: Retreatment vs Apicoectomy Clinical Scenario Retreatment Apicoectomy Missed canals Yes No Blocked post No Yes Prior retreatment failed Usually no Yes Large periapical lesion Depends on access Yes Fractured instrument Maybe Often preferred Good coronal seal Retreatment possible Often unnecessary How Modern Tools Improve Success Rates? Old school struggles have now modern solutions, and they are changing success rates in a big way. Here are few examples- CBCT imaging: A systematic review and meta-analysis reported that CBCT has a sensitivity of 94% and specificity of 93.1% in detecting second canals in permanent teeth6. For the second mesiobuccal canal (MB2) in maxillary molars, the sensitivity was even higher at 96.6%, which promises the potential to make “missed canals’ a thing in the past. A study further analysed 208 CBCT scans and found that 40.7% of maxillary first molars had "missed canals". The numbers highlight the prevalence of undetected canals in conventional imaging and emphasise the importance of advanced diagnostic tools7. Magnification: Magnification tools, such as loupes and dental microscopes, make it easier to spot canal openings and perform treatments more precisely. A 2018 review found that using magnification reduces errors and improves overall success in root canal procedures8. Glide path & crown-down techniques: Glide path and crown-down techniques are not just buzzwords; rather, they are essential steps in modern endodontics. Utilizing rotary glide path files like ProGlider has been shown to significantly reduce apical debris extrusion compared to manual methods, which helps with fewer procedural errors and better patient outcomes9. Bioceramic sealers: They are changing the entire game with their superior sealing ability and contribute to better healing outcomes10. It is proven that with the right tech, technique, and timing, even tough cases can turn out just fine. Case Example: What Would You Do? Case: A 42-year-old presents with a symptomatic maxillary molar with a post and crown. CBCT reveals missed MB2 and a periapical lesion. If the post is easily removed and the crown is temporary: -Retreatment. If the post is long, cast, and removal may cause fracture: -Surgery may be the safer route. Final Thoughts There is no straightforward answer to opt for retreatment or surgery. Both retreatment and surgery are valid evidence-based options. The decision depends on anatomy, restorability, patient factors, and clinician experience. Use a structured approach acknowledging clinical, radiographic, and patient-centered aspects to select the most predictable option. References Aljabri MK, Kensara JA, Mandorah AO, Sunbul MA. Causes of root canal treatment failure: A prospective study in Makkah City, Saudi Arabia. Saudi J Oral Sci. 2020;7(1):40–45. Siqueira JF Jr, Rôças IN, Ricucci D, Hülsmann M. Causes and management of post-treatment apical periodontitis. Br Dent J. 2014 Mar;216(6):305–312. Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009 Jul;35(7):930–7. Setzer FC, Kratchman SI. Present status and future directions: Surgical endodontics. Int Endod J. 2022;55(Suppl. 4):1020–1058. Song M, Kim E, Kim RH, Lee SJ, Kim Y. Prognostic factors of clinical outcomes in endodontic microsurgery: a retrospective study. J Endod. 2011;37(7):927–33. Aung NM, Myint KK. Diagnostic accuracy of CBCT for detection of second canal of permanent teeth: A systematic review and meta-analysis. Int J Dent. 2021;2021:1107471. Alotaibi BB, Khan KI, Javed MQ, Dutta SD, Shaikh SS, Almutairi NM. Relationship between apical periodontitis and missed canals in mesio-buccal roots of maxillary molars: CBCT study. J Dent Sci. 2023;18(3):1034–1040. Low JF, Mohd Dom TN, Baharin SA. Magnification in endodontics: A review of its application and acceptance among dental practitioners. Eur J Dent. 2018 Oct–Dec;12(4):610–616. Akhlaghi NM, Aminsobhani M, Ghandi M, Norouzi N. Effect of different glide path establishing techniques on apical debris extrusion using two single-file systems: an in vitro study. Endodontology. 2023;35(4):123–130. Zhang W, Li Z, Peng B. Assessment of a new root canal sealer's apical sealing ability and biocompatibility. J Endod. 2009 Jun;35(6):915–918.
Article
Latest Irrigation Protocols in Endodontics That Improve Root Canal Treatment Success
Shaping the canal is the most discussed aspect, but we often overlook the crucial role of irrigation in root canal success. Irrigants work their magic by dissolving necrotic tissue, disrupting resilient biofilms, and removing the smear layer that mechanical files leave behind. Advances in irrigation protocols have revolutionized endodontics by improving disinfection efficacy and treatment predictability. Why Irrigation Is Critical in Root Canal Therapy? Root canals come with accessory canals, lateral canals, isthmuses, and dentinal tubules that files alone cannot reach. Failure to adequately disinfect these areas significantly contributes to endodontic failure1. Core Components of the Latest Irrigation Protocol Sodium Hypochlorite (NaOCl): The Cornerstone Irrigant Sodium hypochlorite continues to be the most effective irrigant due to its broad-spectrum antimicrobial action and ability to dissolve necrotic tissue. Contemporary protocols recommend concentrations between 2.5% and 5.25%, balancing antimicrobial potency and biocompatibility2. It is important to note that higher concentrations improve tissue dissolution but increase cytotoxicity risk, which emphasizes the need for controlled delivery. EDTA and Smear Layer Removal The smear layer, formed during instrumentation, often occludes dentinal tubules and harbors bacteria. A 17% EDTA solution applied for 1–3 minutes effectively removes this layer, enhancing irrigant penetration and sealer adaptation. More recently, agents such as QMix, combine EDTA and chlorhexidine to remove the smear layer while simultaneously providing antibacterial action3. Irrigant Activation Techniques Passive irrigation is insufficient for thorough canal debridement. Activation improves irrigant penetration into canal complexities: Passive Ultrasonic Irrigation (PUI): Ultrasonic tips vibrate at 25-30 kHz, creating acoustic streaming and cavitation that enhances debris removal and bacterial reduction. Studies report better canal wall cleanliness with PUI compared to conventional irrigation4. Sonic Activation: Devices such as the EndoActivator provide lower-frequency agitation, effectively increasing irrigant flow and cleaning efficacy in curved and narrow canals5. Laser-Activated Irrigation: Photon-induced photoacoustic streaming (PIPS) utilizes Er:YAG lasers to activate irrigants, facilitating the removal of smear layers and reducing bacterial growth6. Negative Pressure Irrigation (EndoVac): Instead of pushing irrigants forcefully into the canal, EndoVac uses gentle suction to draw the cleaning solution all the way down to the tip of the root. This approach not only reduces the risk of irrigant being pushed beyond the root, which can cause discomfort and complications, but also ensures more effective cleaning, especially in the hard-to-reach apical third of the canal. Studies show that this negative pressure system enhances irrigant flow and helps achieve a cleaner canal without the risk of extrusion7. Optimized Irrigation Sequence The latest evidence supports an alternating irrigation sequence: Irrigation with 2.5–5.25% NaOCl during instrumentation for continuous tissue dissolution and antimicrobial action. Final rinse with 17% EDTA for 1–3 minutes to remove smear layer. Followed by a final flush with NaOCl or sterile saline to clear residual debris. This sequence is critical, as EDTA exposure before NaOCl can diminish NaOCl’s effectiveness due to chemical interactions8. Emerging Irrigants and Adjuncts A few emerging novel irrigants and adjuncts are: MTAD (mixture of doxycycline, citric acid, and detergent) shows effective smear layer removal and antimicrobial properties. A 2024 study found that MTAD exhibited superior residual antibacterial substantivity over 28 days compared to 2% chlorhexidine (CHX) and 2% chitosan, but is limited by antibiotic resistance concerns9. Chlorhexidine gluconate offers sustained antimicrobial action but lacks tissue-dissolving capabilities and may form precipitates when mixed with sodium hypochlorite (NaOCl), which may ultimately affect canal cleanliness. Natural irrigants like neem extract and green tea polyphenols demonstrate antimicrobial effects in vitro but require more clinical validation. Practical Recommendations for Clinicians Use side-vented irrigation needles to reduce the risk of irrigant extrusion and periapical tissue damage. Avoid excessive pressure during irrigation; instead, focus on gentle delivery coupled with activation. Employ ultrasonic or sonic activation wherever feasible to enhance cleaning efficiency, especially in complex canal anatomies. Tailor irrigant concentration and volume to the case complexity and canal morphology. Adhere strictly to recommended irrigant contact times to maximize efficacy without damaging dentinal structures. Final Thoughts The latest irrigation protocols integrate powerful irrigants, innovative activation techniques, and evidence-based sequences to optimize canal disinfection and treatment outcomes. By embracing these advances, clinicians can significantly reduce endodontic failure rates and improve long-term patient prognosis. Reference Iqbal A. The factors responsible for endodontic treatment failure in the permanent dentitions of the patients reported to the College of Dentistry, the University of Aljouf, Kingdom of Saudi Arabia. J Clin Diagn Res. 2016 May 1;10(5):ZC146–ZC148. Ghivari SB, Bhattacharya H, Bhat KG, Pujar MA. Antimicrobial activity of root canal irrigants against biofilm forming pathogens - An in vitro study. J Conserv Dent. 2017 May-Jun;20(3):147–151 Stojicic S, Shen Y, Qian W, Johnson B, Haapasalo M. Antibacterial and smear layer removal ability of a novel irrigant, QMiX. Int Endod J. 2012;45(4):363–371 Guerreiro-Tanomaru JM, Chávez-Andrade GM, de Faria-Júnior NB, Watanabe E, Tanomaru-Filho M. Effect of passive ultrasonic irrigation on Enterococcus faecalis from root canals: an ex vivo study. Braz Dent J. 2015 Jul-Aug;26(4):342-6. Kharouf N, Pedullà E, La Rosa GRM, Bukiet F, Sauro S, Haikel Y, Mancino D. In vitro evaluation of different irrigation protocols on intracanal smear layer removal in teeth with or without pre-endodontic proximal wall restoration. J Clin Med. 2020 Oct 16;9(10):3325 Olivi G, Genovese C, Campagna E, Tempera G, Rapisarda E. Disinfection efficacy of photon-induced photoacoustic streaming on root canals infected with Enterococcus faecalis: an ex vivo study. J Am Dent Assoc. 2014 Oct;145(10):843-8. van der Sluis LW, Versluis M, Wu MK, Wesselink PR. Passive ultrasonic irrigation of the root canal: a review of the literature. Int Endod J. 2007 Jun;40(6):415-26. Vianna ME, Gomes BPFA, Berber VB, Zaia AA, Ferraz CC, de Souza-Filho FJ. In vitro evaluation of the antimicrobial activity of chlorhexidine and sodium hypochlorite. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(1):79–84. Sonisha S, Gaffoor FMA, Gopakumar R, Girish CS, Mohan R, Anoop VN. Comparative evaluation of residual antibacterial substantivity of chlorhexidine, MTAD and chitosan against Enterococcus faecalis in human root dentin: An in vitro study. J Pharm Bioallied Sci. 2024 Apr;16(Suppl 2):S1400–S1403.
Article.jpg)
Why Inferior Alveolar Nerve Blocks Fail and How to Never Miss Again?
Even after following every step -identify the landmarks, angle the syringe just right, inject your LA, and the patient still jumps in pain when you start the prep. Is that correct? You're not alone. Even when performed correctly, Inferior Alveolar Nerve Blocks (IANBs) fail in up to 15–20% of cases involving symptomatic mandibular molars1. And for many clinicians, it feels like those failures come at the worst possible time: a hot tooth, an anxious patient, or a tight schedule. Today, we break down the real reasons why IANBs fail and, more importantly, show you practical, evidence-backed strategies to get your patients numb the first time. Why IANBs Go Wrong? Anatomical Variation Foramen position varies up to 10 mm vertically and horizontally, even between contralateral sides of the same patient 2. Accessory innervation from the mylohyoid, auriculotemporal, or even transverse cervical nerves can bypass the conventional IANB zone. Technique & Needle Placement Too shallow, anterior/posterior, or incorrect angulation leads to missed deposition3. Dense Cortical Bone Thick mandibular cortex slows diffusion. Even a perfectly placed 1.8 mL may remain trapped in soft tissue. Inflammation & Low pH Inflamed pulps lower pH, shift lidocaine into ionized form and reduce nerve penetration. 7 Practical Solutions to Boost Your Block Success Here are 7 easy and effective ways to combat IANB failures - 1. Switch to Gow-Gates or Akinosi Blocks Gow-Gates Mandibular Nerve Block Why it works? Deposits anesthetic at the neck of the condyle, proximal to all V3 branches, ensuring more complete nerve trunk coverage. Key steps: Have the patient open wide; identify the intertragic notch in the corner of the mouth line. Insert a long needle just distal to the maxillary second molar cusp, aiming upward toward the tragus. Advance until you contact bone (~25 mm), aspirate, then slowly inject 1.8 mL LA over 60 sec. 91–95% success shown in irreversible pulpitis cases, which outperforms the standard IANB4. Akinosi-Vazirani Closed-Mouth Block Why it works? Accesses the pterygomandibular space without requiring mouth opening or bone contact, ideal for trismus or difficult landmarks5. Key steps: Keep mouth lightly closed; locate the mucogingival junction above the maxillary third molar area. Insert the needle parallel to the occlusal plane, advancing ~20 mm into the soft tissue between the ramus and tuberosity. Aspirate, then deposit 1.8 mL LA slowly. Clinical data show that the closed-mouth Akinosi–Vazirani block can achieve success rates up to ~96–97%, comparable or superior to both traditional IANB and Gow‑Gates, and is easier to perform in limited-opening situations6. 3. Supplement with Articaine Buccal Infiltration Articaine’s thiophene ring improves lipid solubility and bone penetration. This is especially valuable in cases with dense cortical bone, where infiltration enhances pulpal anaesthesia. A 1.7 mL buccal infiltration of 4% articaine after IANB boosts success from 57% to 94%, in mandibular molars7. 4. Buffer Your Lidocaine Add sodium bicarbonate (1 part 8.4% to 10 parts lidocaine with epinephrine) to reduce injection pain and accelerate onset by up to 1–2 minutes. Buffering may offer improvements in efficacy, particularly in inflamed tissue, but the primary benefits are improved patient comfort and quicker anesthetic onset8. 5. Pre-Warm Your Cartridge Warming LA to 37 °C decreases patient discomfort and accelerates diffusion kinetics, often leading to a faster, more reliable nerve block onset. 6. Intraosseous or PDL Injection Rescue Intraosseous injection provides a significantly faster onset of anesthesia (1.8 minutes vs. 5.2 minutes) and a higher success rate (91.4% vs. 62.9%) than conventional IANB9. IOI is a highly effective primary or supplemental anesthetic technique in challenging cases requiring rapid and reliable anesthesia. Stabident and X-Tip intraosseous systems deliver local anesthetic directly into cancellous bone, with success rates over 90% in “hot tooth” cases where conventional blocks fail10. Periodontal ligament (PDL) injections, especially when administered with computer-controlled devices like The Wand, provide rapid, reliable supplemental anesthesia and serve as valuable adjuncts during challenging cases. 7. Confirm with Objective Testing Dental practitioners can always run a quick test: Lip numbness ≠ pulpal anesthesia. Use cold testing or EPT to verify the block before drilling. These quick, reliable tests ensure the block is effective and help prevent patient discomfort during procedures. Final Takeaway IANB failures are common but fixable.With the right techniques and tools, you can turn frustrating misses into consistent success. References Lee CR, Yang HJ. Alternative techniques for failure of conventional inferior alveolar nerve block. J Dent Anesth Pain Med. 2019;19(3):125–34. Blanton PL, Jeske AH. The key to profound local anesthesia: neuroanatomy. J Am Dent Assoc. 2003;134(7):753–60. Chakranarayan A, Mukherjee B. Arched needle technique for inferior alveolar mandibular nerve block. J Maxillofac Oral Surg. 2013 Mar;12(1):113–6. Sarfaraz I, Pascoal S, Macedo JP, Salgado A, Rasheed D, Pereira J. Anesthetic efficacy of Gow-Gates versus inferior alveolar nerve block for irreversible pulpitis: a systematic quantitative review. J Dent Anesth Pain Med. 2021 Aug;21(4):269–282. Malamed SF. Handbook of Local Anesthesia. 7th ed. St. Louis: Elsevier; 2019. Ravi Kiran BS, Kashyap VM, Uppada UK, Tiwari P, Mishra A, Sachdeva A. Comparison of efficacy of Halstead, Vazirani–Akinosi and Gow Gates techniques for mandibular anesthesia. J Maxillofac Oral Surg. 2018 Dec;17(4):570–575. Kanaa MD, Meechan JG, Corbett IP, Whitworth JM. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. J Endod. 2006 Oct;32(10):919–23. Guo J, Yin K, Roges R, Enciso R. Efficacy of sodium bicarbonate buffered versus non-buffered lidocaine with epinephrine in inferior alveolar nerve block: A meta-analysis. J Dent Anesth Pain Med. 2018;18(3):129–142. Kumar KC, Bhattarai BP, Subedi S. Comparison of intraosseous injection vs conventional IANB: meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;133(2):e33–e42. American Association of Endodontists. Intraosseous anesthesia with the Stabident® and X‑Tip® systems. Endod Colleagues Excell [Internet]. 2009 Winter.
Article
Local Anesthesia Success in Infected & Inflamed Cases
Local anesthesia (LA) can be frustratingly unreliable in cases of infected or inflamed dental tissues. Even with perfect technique, a standard nerve block may fall short and sometimes last less than half the time. Why? Inflamed tissues change everything. They lower pH, increase blood flow, and alter nerve channel expression. Nevertheless, there is a smarter, evidence-based approach that helps you overcome these biological roadblocks and achieve predictable anaesthesia. Let’s jump to a 5-step strategy that combines pharmacology, technique, and modern science to boost your success to over 90%. Why Inflammation Disrupts Local Anesthesia? First things first, here is why inflammation changes the effects of LA - Acidic pH (≈6.0–6.5): Inflammation lowers tissue pH, which traps most anaesthetic molecules in their ionized form. These charged particles can't easily cross nerve membranes, which reduces anaesthetic penetration. Oxidative Stress: Inflamed tissues generate peroxynitrite, a reactive nitrogen species that alters nerve channel function and disrupts how anesthetics bind. It also reduces membrane stability, further decreasing LA effectiveness1. Resistant Sodium Channels: Inflamed pulps express higher levels of tetrodotoxin-resistant sodium channels. These require stronger or longer-acting anesthetics to block effectively. Increased Blood Flow (Hyperemia): Vasodilation from inflammation flushes anesthetic away, which shortens duration and impacts overall potency. These changes explain why a single standard block often fails and why combining pharmacologic priming, buffering, and targeted delivery can rescue it. The Secret Behind Local Anaesthetic Success Here is how you can ensure effective LA in every case - Step 1: Pre-Treatment Medication NSAID + Acetaminophen (60 min before procedure) Ibuprofen 600 mg + Acetaminophen 500 mg Reduces peripheral sensitization and improves anesthetic efficacy Ibuprofen (600 mg) taken 1 hour before IANB raised success to 78%, compared to 32% with placebo2. Optional: Dexamethasone (8 mg PO) Reduces cytokine release and tissue edema The addition of dexamethasone resulted in significantly better results3. Optional: Antioxidant Support Vitamin C (500–1000 mg), or N-acetylcysteine (600–1200 mg) is known to reduce inflammation and oxidative stress in periodontal tissues, and support healing4. Step 2: Use Buffered or Longer-Acting Agents Buffered Lidocaine (Chairside mix): Mix 10 mL of 2% lidocaine with 1 mL of 8.4% sodium bicarbonate Raises pH to ~7.2 Less injection pain, quicker onset, and deeper anesthesia, especially useful in difficult or inflamed cases5. Use within 1–2 min after mixing due to short shelf life. Longer-Acting Options: Bupivacaine 0.5% or Ropivacaine 0.5–0.75% (plain) - Greater lipid solubility and sodium channel binding - Longer duration and better efficacy in inflamed tissues Commercial Buffering Kits: Simplify pH adjustment at chairside without manual mixing Step 3: Block + Buccal Rescue with Articaine Primary Block: Deliver slowly over 90–120 seconds to reduce back-pressure pain and improve anesthetic spread in inflamed tissues. Rescue Buccal Infiltration (at 5 minutes): Articaine 4% with 1:100,000 epinephrine, 1.7 mL buccally. The thiophene ring enhances bone penetration Proven to boost mandibular molar anesthesia success when the primary block is incomplete6. Step 4: Local Targeted Delivery PDL (Intraligamentary) Injection Volume: Inject ~0.2 mL per root Onset ~60 seconds Supplemental success rates between 50–96% in inflamed mandibular teeth7. Intraosseous (IO) Injection Method: Use devices like Stabident® or X‑Tip® for delivery into cancellous bone. Direct delivery provides onset <30 seconds. Success rates of 86% to 91% have been reported8. Duration is very good for the endodontic treatment appointment. Mepivacaine 3% plain also minimizes systemic effects, including tachycardia, compared to vasoconstrictor-containing solutions. Step 5: Reinforcement & Real-Time Feedback Double-Cartridge (if needed): If the first cartridge provides incomplete anesthesia, slowly deliver a second one. Increases depth and duration of block, especially valuable in partial failures Monitor Continuously: Recheck every 2–3 min: - Lip numbness - Blanching - Patient sensation If discomfort persists, escalate to PDL, then Intraosseous Summary Protocol Step Action Pre-Medicate NSAID + acetaminophen ± dexamethasone ± antioxidant Select Agent Buffered lidocaine or switch to bupivacaine/ropivacaine Initial Block Primary → add articaine buccal at 5 min Rescue Strategy PDL → Intraosseous (mepivacaine plain if needed) Reinforce Double cartridge or alternate block route Final Takeaway Inflammation changes the game, but it doesn’t have to beat you. By layering these strategies like anti-inflammatory priming, pH-adjusted agents, longer-acting anesthetics, and targeted delivery, you can consistently achieve deep anesthesia in even the most challenging cases. References Tsuchiya H. Dental anesthesia in the presence of inflammation: pharmacological mechanisms for the reduced efficacy of local anesthetics. Int J Clin Anesthesiol. 2016 Oct 1;4(3):1059 Parirokh M, Ashouri R, Rekabi AR, Nakhaee N, Pardakhti A, Askarifard S, Abbott PV. The effect of premedication with ibuprofen and indomethacin on the success of inferior alveolar nerve block for teeth with irreversible pulpitis. J Endod. 2010;36(9):1450–4. Yadav G, Sahni A, Srivastava A, Rizvi A, Yadav M. Efficacy of dexamethasone added to 2% lignocaine with 1:80,000 epinephrine on inferior alveolar nerve block in patients with symptomatic irreversible pulpitis: A double-blind randomized clinical trial. J Dent Anesth Pain Med. 2022;22(4):277–85. Ruzijevaite G, Acaite E, Jagelaviciene E. Therapeutic impact of ascorbic acid on oral and periodontal tissues: a systematic literature review. Medicina. 2024;60(12):2041. Goodchild JH, Donaldson M. Novel direct injection chairside buffering technique for local anesthetic use in dentistry. Compend Contin Educ Dent. 2019 Jul-Aug;40(7):e1–e10. Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endod J. 2009;42(3):238–46. Friedman MJ, Hochman MN. Anesthetic Effectiveness of the Supplemental Intraligamentary Injection Administered with a Computer‑Controlled Local Anesthetic Delivery System in Patients with Irreversible Pulpitis. Compend Contin Educ Dent. 2005;26(10 American Association of Endodontists. Intraosseous anesthesia: Clinical update. Endodontics: Colleagues for Excellence. Winter 2009
Article
The Hot Tooth Playbook (No More Guesswork)
A ‘hot tooth’ refers to a symptomatic, inflamed pulp, often in irreversible pulpitis that resists conventional local anaesthesia. These cases are a true test of your anaesthetic strategy. Inflamed tissues lower pH, sensitize nociceptors and create accessory pathways. So, what works across difficult cases of symptomatic irreversible pulpitis? Let’s find out. Why Standard Blocks Often Fail in Hot Tooth? Inflamed pulp = anaesthetic resistance. Lower pH and altered nerve conduction in inflamed tissues make it harder for local anaesthetics to penetrate and numb effectively. Here is how blocks act differently for a hot tooth. Mandibular IANB (conventional): success plummets to 44–56% in irreversible pulpitis vs. ~85% in other cases1. Gow-Gates & Vazirani-Akinosi: yield ~76–93% in non-inflamed cases, but drop similarly in hot molars due to the same pathophysiology. PSA block for maxillary molars: 77–95%, accessory innervation can reduce to ~75% in pulpitis2. ASA/infraorbital (canines/premolars): ~80–92% success, but thinner bone aids infiltration alone in many cases. What Works For Hot Tooth? Articaine Infiltration: The Universal Adjunct Articaine’s thiophene ring improves lipid solubility and bone penetration, giving it a critical edge in hot teeth. Clinical Impact A meta-analysis of 62 trials found that Articaine infiltration is 3.6 times more likely than lidocaine to produce pulpal anaesthesia in hot teeth1. For mandibular cases: Articaine doesn’t outperform lidocaine in the block itself. But for supplemental buccal infiltration, it has a significant advantage. In the maxilla: Buccal articaine infiltration significantly improves success over lidocaine3. Onset & Duration Onset: Articaine = 6–7 min; Lidocaine = 9–10 min. Duration: Articaine = ~25 min (vs. Lidocaine ~50 min), but adequate for most endo access Does More Volume Help? The 1.8 mL vs. 3.6 mL Articaine Debate A common clinical question when managing “hot teeth” with symptomatic irreversible pulpitis is whether increasing the volume of anaesthetic improves success. A randomized clinical trial put this to the test by comparing 1.8 mL versus 3.6 mL of 4% articaine (1:100,000 epinephrine) for inferior alveolar nerve block (IANB) and supplemental periodontal ligament (PDL) injections. Here’s what they found: IANB success in pulpal anaesthesia was 27% for 1.8 mL vs. 42% for 3.6 mL, which was not statistically significant4. Pain-free pulpectomy was achieved in 64% vs. 73%, respectively. PDL injection “rescue” success was 75% with 1.8 mL, but only 42% with 3.6 mL, again not statistically significant. Therefore, increasing the volume of articaine doesn’t significantly boost success in hot teeth cases. Using more anaesthetic doesn’t necessarily result in better outcomes; clinicians should focus on technique, not just volume. Supplemental “Rescue” Techniques When All Else Fails If the block + infiltration combo doesn't provide full anaesthesia, escalate strategically: Periodontal Ligament (PDL) Injection Adds anaesthesia in 69–75% of failed-block cases. Useful regardless of the initial block technique. Intraosseous (IO) Injection Delivers direct access to cancellous bone vasculature. Success: 88% overall (91% mandible, 67% maxilla). Systems: X-Tip, Stabident. Intrapulpal Injection Nearly 100% effective—but painful. Requires back pressure and is best used as a last resort when the pulp chamber is already accessed. Protocol Cheat Sheet: Best Practices by Region Clinical Scenario Recommended Approach Mandibular hot molar IANB (Gow-Gates/Vazirani optional) + 4% Articaine buccal infiltration Maxillary molars PSA block + buccal Articaine infiltration; add palatal or IO as needed Anterior maxilla/premolars ASA or AMSA + buccal infiltration; consider palatal block for supplement Still painful post block + infiltration Add PDL or IO injection; reserve intrapulpal as the final step Key Takeaways: Building a Predictable Anaesthetic Strategy Never rely solely on nerve blocks in inflamed teeth. Supplement every block with buccal articaine infiltration; it is your universal enhancer. Use PDL or IO as rescue steps, not as primary approaches. Intrapulpal works, but it is your last resort as it is high on the pain scale. Final Takeaway A hot tooth doesn’t have to mean a hot mess. By understanding why traditional techniques fail and how to layer anaesthesia methods effectively, you can transform challenging pulpitis cases into predictable successes. Stay systematic. Stay evidence-based. Your patients (and your stress levels) will thank you. References Kung J, McDonagh M, Sedgley CM. Does articaine provide an advantage over lidocaine in patients with symptomatic irreversible pulpitis? A systematic review and meta‐analysis. J Endod. 2015;41(12):1784–1794 American Association of Endodontists. Successful Local Anesthesia: What Endodontists Need to Know [Internet]. Chicago: American Association of Endodontists Rogers BS, Botero TM, McDonald NJ, Gardner RJ, Peters MC. Efficacy of articaine versus lidocaine as a supplemental buccal infiltration in mandibular molars with irreversible pulpitis: a prospective, randomized, double-blind study. J Endod. 2014 Jun;40(6):753–8 Silva SA, Horliana ACRT, Pannuti CM, Braz‑Silva PH, Bispo CGC, Buscariolo IA, Rocha RG, Tortamano IP. Comparative evaluation of anesthetic efficacy of 1.8 mL and 3.6 mL of articaine in irreversible pulpitis of the mandibular molar: a randomized clinical trial. PLoS One. 2019 Jul 31;14(7):e0219536. doi:10.1371/journal.pone.0219536.
Article
Buffered Local Anesthesia: Is It Worth the Hype?
Buffering local anesthetic by adding sodium bicarbonate to raise pH is becoming more common among dental clinicians aiming for less pain and faster onset. But does the evidence support making this a routine part of practice? Well, here is a clinically relevant guide based on the latest research. The Science of Buffering Standard lidocaine and articaine cartridges are acidic (pH ~3.5–5.5) to preserve epinephrine. Buffering with sodium bicarbonate raises the pH near physiologic (~7.4), which increases the non-ionized anesthetic available for nerve penetration. This change reduces the "burn" during injection and accelerates the onset1. What Research Shows? A. IANB in Adults Buffered lidocaine achieved faster onset (~48 s) and less injection pain (~5 VAS points) compared to non-buffered options2. However, the success rates of profound anesthesia remained statistically similar. B. Buffered Articaine for Mandibular Infiltration A 2023 clinical trial (63 volunteers) showed buffered 4% articaine had a significantly faster onset (4.5 ± 1.6 min vs. 6.6 ± 1.6 min, P=0.001) and lower injection pain (7.8 mm vs. 11.3 mm VAS, P=0.001), though anesthetic success was comparable3. C. Buffered Articaine in Maxilla A 2015 trial comparing buffered vs. non-buffered 4% articaine for first molar infiltration found no difference in onset or pain, suggesting tissue variability matters4. D. Pediatric Block in Primary Molars Controlled pediatric RCT demonstrated that warmed or buffered 2% lidocaine reduced pain and improved onset/duration in children’s IANBs5. Chairside Buffering: How to Do It? Manual Mixing (Easy DIY): Withdraw about 0.18 mL from a 1.8 mL LA cartridge, replace with 0.18 mL of 8.4% sodium bicarbonate (a 10:1 ratio)6. Mix gently and eliminate air bubbles before injection. Pre‑Buffered Systems: Pre-buffered delivery systems allow chairside buffering of local anesthetics in seconds, without manual mixing or syringe changes. Tools like OnPharma Onset Pen and Anutra streamline the process by incorporating buffering mechanisms directly and improve efficiency and consistency. Practical tips: Use buffered cartridges within 24 hours, as they degrade faster. Always expel air bubbles to prevent any pressure jolts. Streamlined with modern devices, buffering adds only 10–15 seconds of chairside time. When Buffering Makes a Difference? linical Situation Buffer Benefit Worth It? Routine block/infiltration Slightly faster (≈1 min) Optional Inflamed/hot tooth Much faster (≈2 min) ✔️ Recommended Anxious or pediatric patients Noticeably more comfortable ✔️ Highly recommended Volume-oriented clinics Shorter appointments ✔️ Consider Final Takeaway Buffering the local anaesthesia may not guarantee a deeper effect, but it does provide benefits such as faster onset and reduced pain.These benefits are important for inflamed tissues and sensitive patients. Pre-buffered kits offer minimal hassle and position themselves as a smart upgrade for modern practices. References Senthoor P, Janani K, Ravindran C. A prospective, randomized double-blinded study to evaluate the efficacy of buffered local anesthetics in infected and inflamed pulp and periapical tissues. J Maxillofac Oral Surg. 2019;19(2):246–250. Guo J, Li Y, Wang Y, Deng Y. Comparison of buffered and non-buffered lidocaine in inferior alveolar nerve block: a meta-analysis. J Dent Anesth Pain Med. 2018;18(3):129–142. Roodnick S, Chisci G, Mijiritsky E, Salari A, Shpack N. The effect of buffered versus non-buffered 4% articaine with 1:100,000 epinephrine on mandibular first molar infiltration: A randomized, double-blind, crossover clinical trial. J Dent Sci. 2023;18(3):1047–1054. Shurtz R, Nusstein J, Reader A, Drum M, Fowler S, Beck M. Buffered 4% articaine as a primary buccal infiltration of the mandibular first molar: a prospective, randomized, double-blind study. J Endod. 2015 Sep;41(9):1403–1407. Kurien RS, Goswami M, Singh S. Comparative evaluation of anesthetic efficacy of warm, buffered and conventional 2% lignocaine for the success of inferior alveolar nerve block (IANB) in mandibular primary molars: A randomized controlled clinical trial. J Dent Res Dent Clin Dent Prospects. 2018;12(2):102–109. Malamed SF. Buffering local anesthetics in dentistry. J Am Dent Assoc. 2013 Aug;144(8):867–872.
Article