
AI-Assisted Smile Design: The Smart Revolution in Aesthetic Dentistry
Smile design has always required an artistic eye and deep anatomical knowledge.
But today, AI is augmenting that skillset and brings in unprecedented speed, accuracy, and patient engagement to the process.
AI-assisted smile design isn’t science fiction anymore; it is a chairside reality now.
From real-time smile simulations to precision planning aligned with facial anatomy, dentists now have access to tools that make aesthetic cases more predictable and profitable.
But how does it really work? Let’s find out.
What Is AI-Assisted Smile Design?
AI-assisted smile design uses machine learning algorithms to analyze facial and dental data and automates the process of designing an aesthetic smile that matches the patient's natural features.
Unlike traditional Digital Smile Design (DSD), AI tools can:
- Instantly detect over 60 facial and dental landmarks (lip line, midline, interpupillary line, gingival contours, etc.)
- Suggest optimized tooth shapes and positions based on large datasets of successful aesthetic cases.
- Provide dynamic 2D and 3D simulations of treatment outcomes1.
Key Capabilities
- AI-powered tools can identify dental and facial landmarks with approximately 93% accuracy, which makes them far more consistent than manual identification2.
- Smile simulation generation in under 3 minutes.
- Integration with CAD/CAM and lab workflows3.
How Does It Actually Work?
Now that we have you with us, let’s see how the magic happens.
1. Facial & Dental Landmark Detection
AI scans patient photographs or 3D facial scans and identifies anatomical landmarks using convolutional neural networks (CNNs). These include:
- Facial midline, interpupillary line, and smile curve
- Gingival margins and incisal edges
- Buccal corridors and lip symmetry
2. AI-Driven Smile Design Algorithms
AI works on training sets from thousands of aesthetic cases, and suggests tooth shapes and gingival contours that match the patient’s facial typology. Many platforms provide a preloaded digital tooth library.
3. Real-Time Simulations
The system renders a 2D or 3D smile simulation within minutes, which can be customised by either the clinician or the patient. These simulations can be exported directly to labs or printed as mock-ups4.
Clinical Benefits: Why Should You Adopt AI?
Here are a few solid pros you should consider -
1. Speed & Accuracy
Manual digital smile designs can take as long as 45–60 minutes. AI systems reduce this to under 5 minutes with improved precision.
2. Enhanced Case Acceptance
Seeing is believing. Studies show that patients who view their simulations achieved excellent esthetic outcomes compared with 78% in the conventional mock-up group, and they reported higher satisfaction scores5.
3. Seamless Integration with Lab Workflows
Smile files are CAD-ready and compatible with most dental software systems, that helps reduce lab miscommunication and chairside rework.
4. Improved Interdisciplinary Planning
AI-assisted digital smile design platforms now merge CBCT scans, facial surface scans, and intraoral STL models into one 3D ‘virtual patient’.
It gives the dental practitioner a unified treatment plan for restorative, periodontal, and orthodontic needs with sub-millimeter precision, and lets you preview and perfect every aspect of the patient’s new smile before you ever pick up a handpiece.
Limitations: Where AI Still Needs the Human Touch
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
AI enhances, but does not replace, clinical judgment. The clinician’s eye is still essential, especially in complex or interdisciplinary cases.
Top Tools & What to Look For
When choosing an AI smile design platform, consider these features:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Popular Tools: 3Shape Smile Design, DSDApp (by Coachman), Smile cloud, IvoSmile, SmileFy
Final Takeaway
AI isn’t replacing cosmetic dentists; rather, it is empowering them. The blend of human artistry and machine precision means more predictable outcomes, higher patient trust, and faster workflows.
Whether you are a seasoned aesthetic dentist or just getting started with smile makeovers, AI can transform how you plan, present, and perform.
References
- Jreige CS, Kimura RN, Segundo ÂRTC, Coachman C, Sesma N. Esthetic treatment planning with digital animation of the smile dynamics: a technique to create a 4-dimensional virtual patient. J Prosthet Dent. 2022 Aug;128(2):130–138
- Alahmari M, Alahmari M, Almuaddi A, Abdelmagyd H, Rao K, Hamdoon Z, et al. Accuracy of artificial intelligence-based segmentation in maxillofacial structures: a systematic review. BMC Oral Health. 2025 Mar 7;25:350.
- Revilla-León M, Gómez-Polo M, Vyas S, Barmak AB, Özcan M, Att W, Krishnamurthy VR. Artificial intelligence applications in restorative dentistry: a systematic review. J Prosthet Dent. 2022 Nov;128(5):867–875. doi:10.1016/j.prosdent.2021.02.010. PMID: 33840515.
- Chen YW, Stanley K, Att W. Artificial intelligence in dentistry: current applications and future perspectives. Quintessence Int. 2020;51(4):269–280
- Luniyal C, Shukla AK, Priyadarshi M, et al. Assessment of patient satisfaction and treatment outcomes in digital smile design vs. conventional smile design: a randomized controlled trial. J Pharm Bioallied Sci. 2023 Dec;16(Suppl 1):S669–S671.
Related Content

From Dentist to CEO: What Dental College Never Taught You
A dentist spends years mastering root canals, crown preps, and radiographic interpretation. But what about other aspects of running a practice, like revenue optimization, team management, or clinic operations? Dental education in India, even at top institutions, is still heavily focused on clinical proficiency, not practice management. When you set up your clinic, these values become even more relevant. You are no longer just a doctor; you become a business owner. A CEO. And in today’s hyper-competitive dental market, that shift is no longer optional. Why You Must Make the Dentist-to-CEO Shift? In India, over 80% of private dental clinics are solo or small setups. That means the dentist is the business1. However, most clinics plateau at a certain income level. This is not because the dentist isn’t skilled, but simply because the business side is neglected. A 2022 survey of 100 dentists from Chennai revealed that 61% felt practice management should be an integral part of the undergraduate curriculum, and over half believed their practice success would improve if such training were mandatory2. Successful clinic owners treat their practice like a healthcare business: They measure performance They train and retain staff They systemise operations They plan revenue streams proactively If you are only focused on treating patients and keep ignoring finances, systems, and leadership, you will burn out or stagnate. Let’s help you flip the script. 1. Know Your Numbers Run your clinic with data. Start by tracking 5 essential metrics every month3: Metric Ideal Benchmark Monthly revenue per chair ₹2–3 lakhs/chair Case acceptance rate > 60% Patient retention rate > 70% Chair occupancy rate 80%+ Treatment plan conversion > 50% Don’t overcomplicate it. Use a simple Google Sheet or clinic software like: Practo Ray Docpulse Even a basic Excel dashboard can reveal where you are leaking money. 2. Build Systems That Work Without You How much of your day is wasted answering repetitive staff questions, checking appointments manually, or following up on missed payments? These are symptoms of a missing system. Standard Operating Procedures (SOPs) to create: New patient registration & consent process Treatment explanation and fee presentation Lab coordination workflows Sterilisation checklist Post-op and recall communication protocol Pro Tip: Use WhatsApp groups for team SOP reminders, or create short video SOPs on your phone, which makes it easy for new staff to follow. Evidence backs this up: A 2024 Frontiers in Education study recommends structured interprofessional modules in dental education to train students in leadership, systems thinking, and process-driven practice management4. 3. Lead Your Team Like a CEO, Not a Boss The Indian dental workforce is often young, undertrained, and high-churn. That’s why leadership matters more than micromanagement. Your team does not always need you to do everything. They need: Clear roles and daily tasks A growth path Regular appreciation and feedback, which can be a weekly check-in A culture where patients are the priority, not just “completing the case” Action Step: Assign a clinic operations champion, even a part-time one will do. They can handle stock, follow-ups, and non-clinical issues. This frees up your headspace. 4. Take Control of Your Finances Even if you outsource accounting, you should own your numbers. These are key financial insights to track monthly: Gross income vs net profit Staff salaries as a % of revenue (aim for <30%) Lab & material costs (keep under 12–15%) High-value vs low-value procedures (so you market wisely) Along with that, budget monthly for: Equipment maintenance Staff training Marketing (even ₹5,000–10,000/month goes far) Tools you can use: Tally or Zoho Books for basic accounting Your CA can help generate monthly P&L reports. 5. Block Time for CEO Work If you are in the chair from 9 AM to 9 PM, you are working in the business, not on it. You have to block 2 hours a week for CEO tasks like: Reviewing numbers Planning local promotions Meeting vendors, marketers, or legal advisors Researching new tech (e.g. aligners, CAD/CAM, intraoral scanners, AI software) You can always use Google Calendar or Notion to schedule & track. Weekly CEO Routine Task Time Tool Review revenue & new patients 20 min Practice software/Excel Weekly team huddle 15 min In-person/WhatsApp Check inventory & lab coordination 15 min Checklist Marketing brainstorm/outreach 30 min Canva, Google My Business Long-term planning 30 min Notebook/whiteboard Final Takeaway You must believe that you are not just a doctor, but a dental entrepreneur. Clinical skill may bring in patients, but systems, strategy, and leadership are what keep them coming back and grow your income. The best part? You really don’t need an MBA. You need a mindset shift, a weekly discipline, and the willingness to learn what wasn’t taught in dental college. References Multani HS. India’s dental care market: current status and the way forward. Times of India [Internet]. 2021 Sep 9 [cited 2025 Jun 27]. Aathira CM, Jeevanandan G, Govindaraju L. Need for practice management in undergraduate dental program – a cross sectional survey among the dentists. J Adv Pharm Technol Res. 2022 Dec 30;13(Suppl 2):S453–7. American Dental Association. Measuring success: dental practice management. [Internet]. Chicago: ADA; [cited 2025 Jun 27]. Sujir N, Naik DG, Mohammed CA, Jain A, Uppoor A. Introducing dental practice management in the undergraduate curriculum through an interprofessional module: experience from an Indian dental school. Frontiers in Education. 2024; Nov 11

5 Biggest Revenue Leaks in Dentistry and How to Fix Them
Even if a dental practitioner is amazing at spotting a crack in a patient’s tooth, what about the cracks in the dental practice? Many dental practitioners work tirelessly to deliver outstanding clinical care, yet overlook the silent money leaks that drain profitability month after month. Hidden revenue leaks might be to blame. Let’s shed some light on them and stop the drip before it turns into a flood. Leak 1: Inefficient Scheduling and Open Chair Time Industry data show that practices can boost production by up to 25–30% simply by tightening scheduling gaps and reducing no‑shows1. Solution: Audit your past 6 months: track every empty chair slot and measure average patient wait times. Invest in a modern, automated recall and confirmation system. Train your front‑desk team to offer the next available appointment at checkout and don’t wait for patients to call in. Leak 2: Incomplete Treatment Acceptance Even when you present the ideal treatment plan, a significant share of patients never follow through. This means you leave real revenue on the table. In a recent survey of 771 patients recommended for endodontic or restorative therapy, only 68.5 % actually underwent the treatment, which accounts for 30% of lost treatment opportunities2. Solution: Use high-impact visuals and before-and-after case photos in every consultation. Practice mock consultations with your team so they can smoothly turn around “I’ll think about it” statements. Offer flexible payment plans, such as in-house financing or third-party options, to remove cost barriers. Leak 3: Outdated or Ineffective Fee Structures Henry Schein’s Fee Balancing (HSPA) analysis demonstrates that practices that update their fees every 12 months can see an increase of almost 8–15 per cent in annual revenue, simply by aligning fees with market percentiles and inflation3. Solution: Benchmark your fees annually against regional and national data. Communicate fee changes clearly and focus on the value and quality you deliver, not just the price. Bundle popular services (e.g., hygiene + periodic exam) into preventive‑care memberships. Leak 4: Insurance Overdependence and Write‑Offs While only an estimated 10–15 per cent of Indian dental patients carry any form of dental rider on their health insurance policies. Practices that accept and process these claims still see around 25 per cent of billed amounts written off due to non-covered procedures, claim rejections, or administrative errors4. Solution: Run a 90‑day claim audit. Identify the insurers and procedure codes with the highest rejection rates and tighten your submission protocols. Educate patients and clearly explain which services are and aren’t covered, so they are prepared for out‑of‑pocket costs rather than surprised by a write‑off. Streamline your hybrid model. Consider accepting only a select few plans with reasonable coverage and fast turnaround, and promoting fee‑for‑service for treatments outside those networks. Leak 5: Missed Opportunities for Ancillary Services Data from the Journal of the American Dental Association show that practices actively marketing cosmetic and wellness services see a 15–20% uplift in ancillary revenues within a year5. Solution: Train your hygiene team to flag cosmetic concerns (staining, minor misalignment) and discuss options. Create simple, in‑office brochures and digital content on whitening, clear aligners, and wellness plans. Run periodic “smile makeover” events or limited‑time offers to drive patient interest. Final Takeaway Plugging revenue leaks isn’t about squeezing more out of patients, it’s about delivering more value and getting paid fairly for the quality you provide. Start small, pick one leak to address this month, and you will see steady growth in both revenue and patient satisfaction. References Levin RP. Higher production and long‑awaited stability: The 2024 DE/Levin Group Annual Practice Survey [Internet]. Dent Econ; 2024 May 8[cited 2025 Jul 1] Mohan S, Viswanath B, Kumar G, Priyank H. Questionnaire‑Based Assessment of Patients’ Knowledge, Attitude, and Practices Regarding Restorative and Endodontic Treatment at a Multi‑disciplinary Tertiary Care Hospital of Jharkhand, India [Internet]. Cureus. 2024May 2;16(5):e59526. Henry Schein Dental. Fee Balancing: How Annual Fee Schedule Reviews Drive 8–15 Percent Revenue Growth [Internet]. Dental Practice Transitions; 2023. Insurance Regulatory and Development Authority of India. Annual Report 2022–23 [Internet]. Mumbai: IRDAI; 2023. American Academy of Cosmetic Dentistry. AACD 2022 State of the Cosmetic Dentistry Industry Survey. Dentistry Today [Internet]. 2022 Nov 3 [cited 2025 Aug 27]

Practical Playbook to Cut Dental No-Shows by 30%
No-shows aren’t just empty chairs, they disrupt schedules, frustrate teams, and dent your practice income. With smart strategies, it’s possible to reduce no-shows by up to 30%, making your practice more efficient and patient-friendly. Why Patients Often Don’t Show Up? Common reasons for patients to miss their appointment include: Forgetting the appointment Perceiving dental care as non-urgent Scheduling conflicts Cost-related anxiety What Should You Do to Reduce No-Shows? Here are six solid points that can help you reduce the no-shows and run an efficient practice. 1) Upgrade reminders: timing, channel, and content Simple reminder systems work, but structured, timely reminders work better. A 2019 meta-analysis in orthodontics found electronic reminders were associated with substantially lower missed visits compared with no reminders, highlighting the impact of consistent digital nudges1. Do this: Send two reminders (e.g., 72–48 hours and 24 hours before the visit). Use SMS as default; add email/voice for patients who opt in. Keep messages short, include clinic name, date/time, location map link, and a one-tap confirm/reschedule option. Add a clear “Please reply C to confirm or R to rebook” Two-way texting improves actionability. 2) Make rescheduling effortless and fast When rescheduling is frictionless, patients are less likely to become no-shows. In a 2021 randomized trial across >140,000 primary-care appointments, targeted text reminders increased confirmations and attendance versus standard practice2. Do this: Offer self-serve rescheduling from the reminder (no portal login required). Keep a live waitlist; when someone cancels via text, auto-offer the slot to waitlisted patients. 3) Use data to predict risk (and over-protect those slots) Machine-learning models can help identify higher-risk bookings like long lead times, late-day slots, and prior no-shows. Reviews show predictive tools help clinics proactively overbook or add extra reminders to high-risk slots without increasing congestion3. Do this: Tag “high-risk” criteria like first-time visitors, long lead time, and history of no-shows. Add an extra reminder and earlier follow-up call for those bookings. For chronically missed low-acuity visits, consider light overbooking guided by your data. 4) Shorten lead times and right-size slots Long delays between booking and visit can be the reason for non-attendance. Operations research consistently links shorter wait times and appointment lengths that are right-sized to fewer no-shows and improved throughput. Do this: Hold back same-week capacity for high-demand services like whitening or aligner checks. Audit procedures: If 40-minute checks regularly finish in 25, shrink the template and add a buffer rather than booking long by default. 5) Set clear expectations without alienating patients Clear policies reduce last-minute cancellations, but a heavy-handed approach can also backfire. Always pair a friendly policy with supportive messaging: “We reserve this time for you. If you need to change it, please reply or call; someone on our waitlist will be grateful.” Do this: Share your cancellation window in every reminder. For repeated no-shows, consider switching to shorter lead times, morning slots, or implementing pre-visit confirmation calls. 6) Offer virtual where appropriate For short checks or consults, tele-appointments often see higher completion rates than in-person during access constraints. Many systems report improved attendance when travel/time barriers drop4. Do this: Shift routine follow-ups and minor consults to virtual visits, and reserve chair time for procedures. What to implement this week? Dual SMS reminders (48–72h and 24h) with one-tap reschedule. Waitlist text fill-ins for cancelled slots. Add risk tags and include an extra reminder & confirmation call. Template audit to shorten chronically over-booked procedures. Kind but clear cancellation message in every reminder. Final Takeaway Cutting no-shows isn’t about complicated systems, it’s about smart reminders, easy rescheduling, and meeting patients where they are. Even small changes like dual SMS reminders, a waitlist, and offering virtual check-ins can reduce missed visits by 30% and keep your schedule full. References Mohammed A, Rizk MZ, Wafaie K, Ulhaq A, Almuzian M. Reminders improve oral hygiene and adherence to appointments in orthodontic patients: a systematic review and meta-analysis. Eur J Orthod. 2019 Mar 29;41(2):204–213. Ulloa-Pérez E, Blasi PR, Westbrook EO, Lozano P, Coleman KF, Coley RY. Pragmatic randomized study of targeted text message reminders to reduce missed clinic visits. Perm J. 2022 Apr 5;26(1):64–72. Deina C, Fogliatto FS, da Silveira GJC, Anzanello MJ. Decision analysis framework for predicting no-shows to appointments using machine learning algorithms. BMC Health Services Research. 2024;24(1):37. Cummins MR, Tsalatsanis A, Chaphalkar C, Ivanova J. Telemedicine appointments are more likely to be completed than in-person healthcare appointments: a retrospective cohort study. JAMIA Open. 2024 Jul;7(3):ooae059.

Teeth Whitening Trends You Cannot Ignore: A 2025 Guide for Dentists
Teeth whitening remains a top-requested cosmetic procedure, with an ever-increasing patient demand for fast, safe, and long-lasting results. As dental professionals, staying updated on whitening technologies, clinical protocols, and patient-centric strategies is essential for delivering both aesthetic and functional excellence. In‑Office Whitening: Still the Gold Standard Uses high‑concentration hydrogen peroxide (25–40%), which is further often accelerated with lasers or LEDs, to lighten teeth by multiple shades in under an hour. Clinical trials show similar whitening efficacy and sensitivity across concentrations (18%, 25%, 40%) with improvements in aesthetic perception at 6 months1. Light-activated systems (laser or LED) boost efficacy while limiting exposure time . Best practices: Pre‐treatment assessment: Evaluate shade, sensitivity risk, and expectations. Professional isolation: Use rubber dams or trays to protect soft tissues. Customize protocol: Choose gel concentration and light source based on factors such as history of fluorosis, presence of restorations, or intrinsic stains that may require more advanced or repeated treatment Manage sensitivity: Incorporate desensitizing agents like potassium nitrate or fluoride during treatment2. Contraindications: In-office whitening is not recommended for patients with conditions such as pregnancy, those under 16 years of age, untreated caries or periodontal disease, or multiple restorations in the aesthetic zone. Always complete a thorough oral evaluation before recommending whitening. Follow-up and maintenance: A post-treatment take-home kit or maintenance app can prolong results. Take‑Home Kits & Hybrid Models Dentist‑prescribed kits with 10‑35% carbamide peroxide or 6‑10% hydrogen peroxide remain effective with less chair time2. LED-accelerated at-home kits deliver gradual yet consistent results, which is ideal for maintenance following in-office sessions. Hybrid protocols (in‑office + at‑home) maintained significantly whiter teeth even 2 years later. This proves that hybrid protocols aren’t just convenient, they are clinically superior for long-term brilliance3. Implementation tips: Provide 3D‑printed custom trays for better fit and comfort. Educate patients: 1–4 weeks of at-home use vs. a one-off in-office session. Consider incorporating AI-based shade matching apps or intraoral cameras for consistent baseline and outcome tracking. Emerging Technologies & Ingredients Here are latest trends in the teeth whitening space - Laser-activated bleaching: Offers gentler, more efficient results in minutes. Violet LED & infrared photobiomodulation: Studies show reduced sensitivity and faster bleaching4. Smart Bleaching Systems: New AI-driven systems auto-adjust bleaching light wavelength and intensity based on real-time shade detection, which offers a customized and efficient approach. These are promising but may come at higher setup costs. Peroxide-free agents (PAP): Popular for sensitive patients; plant-based, enamel-friendly, but still needing stronger clinical validation5. Sensitivity Management Transient sensitivity is a common post-treatment effect, reported by almost 70% of the patients6. Use desensitising options pre/post-bleaching like fluoride, potassium nitrate, and ACP. Recommend the use of high-fluoride trays (e.g., 5000 ppm fluoride) post-bleaching to reduce tubule permeability and support enamel remineralization. Schedule follow-up sensitivity checks within 48–72 hours, especially for patients with a prior history of post-op discomfort. Choose neutral‑pH gels, include sensitivity protocols, and offer professional-strength remineralizing toothpaste. Longevity & Maintenance Color relapse typically occurs within 6–12 months; combined or at-home boosters mitigate this. Educate patients to avoid staining foods/drinks and to schedule regular cleanings. Offer subscription whitening plans (e.g., biannual in-office + take-home) to improve long-term retention and revenue. Patient Education & Marketing Debunk myths, e.g., DIY hacks with charcoal or lemon which are commonly practised. Explain the enamel risks with supporting evidence . Leverage Digital Smile Design and shade simulations to set realistic goals and improve acceptance. Promote whitening as part of a full aesthetic package and emphasize the synergy with veneers, bonding, and soft tissue aesthetics. Final Takeaway In-office whitening remains the fastest and most predictable solution, but today’s most successful practices blend evidence-based protocols with smart technology, long-term maintenance strategies, and personalized sensitivity care. By integrating these trends, clinicians not only enhance patient satisfaction but also position whitening as a valuable, recurring revenue stream within the broader scope of cosmetic dentistry. References Altınışık H, Nezir M. Clinical evaluation of in‑office bleaching with low, medium, and high concentrate hydrogen peroxide: a 6‑month double‑blinded randomized controlled trial. Clin Oral Investig. 2025 Apr 21;29(5):260. doi:10.1007/s00784-025-06348-8. Kury M, Bem Prunes B, Saraceni CHC, Hilgert LA, Fronza BM, Lima AF. Clinical decision‑making in tooth bleaching based on current evidence: A narrative review. Dent Mater. 2025 May;41(5):536–52. Takamizawa Y, Kato T, Nara Y, Iwasa A, Irokawa T, Ando Y, et al. Long-term color stability of in-office bleaching with or without at-home tray bleaching: a double-blind randomized clinical trial. J Esthet Restor Dent. 2025 Jun;37(4):561–8. dos Santos AECG, Bussadori SK, Pinto MM, Pantano Junior DA, Brugnera A Jr, Zanin FAA, Rodrigues MFSD, Motta LJ, Horliana ACRT. Evaluation of in‑office tooth whitening treatment with violet LED: protocol for a randomised controlled clinical trial. BMJ Open. 2018 Sep 4;8(9):e021414 Pascolutti M, de Oliveira D. A radical‑free approach to teeth whitening: in vitro evaluation of a novel PAP+ gel formulation. Dent J (Basel). 2021 Dec 9;9(12):148. Martini EC, Parreiras SO, Szesz ALS, Coppla FM, Loguercio AD, Reis A. Bleaching-induced tooth sensitivity with application of a desensitizing gel before and after in-office bleaching: a triple-blind randomized clinical trial. Clin Oral Investig. 2020 Jan;24(1):385–394.

Soft Tissue Aesthetics in Dentistry: Beyond the Smile Line
When we think of smile aesthetics, our focus often stops at teeth, their shade, shape, alignment are all we think of. But without balanced gums and lips, even the whitest, straightest teeth can look incomplete. Soft tissue aesthetics can elevate a good smile makeover into a truly harmonious result. From subtle gingival contouring to complex peri-implant tissue management, advances in minimally invasive techniques now enable clinicians to achieve both health and beauty in a single procedure1. So, what does soft tissue aesthetics involve, and how can it maximize patient satisfaction and practice revenue? Let’s explore. What Is Soft Tissue Aesthetics? Soft tissue aesthetics refers to the enhancement and management of gingival and peri-oral tissues to complement dental restorations or natural dentition2. Key goals may include: Creating gingival symmetry and harmony with teeth Managing excessive gingival display (“gummy smile”) Establishing natural-looking papillae around implants or crowns Achieving lip–tooth balance in repose and during a smile Core Techniques in Soft Tissue Aesthetics Here are the core techniques you should be aware of - Gingival Contouring & Crown Lengthening Tools: scalpels, electrosurgery, or dental lasers Application: correct uneven gingival margins or excessive gum display Evidence: minimally invasive approaches show comparable esthetic outcomes with faster healing3 Soft Tissue Grafting Techniques: connective tissue grafts, collagen matrices Purpose: manage gingival recession, provide root coverage, restore natural contours1 Minimally Invasive Laser Techniques Benefits: Lasers (diode, erbium) allow bloodless contouring, reduced postoperative discomfort, and quicker healing Often combined with restorations for immediate esthetic enhancement Peri-implant Tissue Management Essential for long-term success and esthetic stability Strategies: papilla preservation, tissue thickening to achieve a natural emergence profile4 Lip Repositioning & Adjunctive Therapies Minimally invasive surgery can reposition gummy smiles due to hyperactive upper lips Combined crown-lengthening and lip repositioning cases show significant improvements5 Adjuncts: Botox and dermal fillers are increasingly used as dental adjuncts for perioral aesthetics Clinical Benefits: Why Soft Tissue Matters? Here is why you should pay equal attention to soft tissue - Improved Symmetry & Proportion → Harmonizes the smile line with facial features Increased Case Acceptance → Patients perceive a “complete” makeover, not just whiter teeth Long-Term Stability → Healthy soft tissue ensures restorations look natural over time Revenue Growth → Add-on services like gum contouring or lip enhancements increase per-patient value Beyond clinical outcomes, improving soft tissue aesthetics often enhances patients’ self-esteem and quality of life. Limitations & Considerations While techniques are advancing, clinicians must balance aesthetic goals with biological health. Over-contouring can compromise periodontal support Some cases (severe gummy smiles, lip incompetence) may need interdisciplinary planning with orthodontists or plastic surgeons Patient expectations must be managed carefully, as results depend on both tissue biology and surgical skill Tools & What to Look For? When building a soft tissue aesthetics offering, dentists should focus on: Dental lasers for predictable contouring with minimal bleeding Biologic grafting materials like xenografts, collagen matrices, and growth factors for natural tissue architecture Digital planning tools for integrating smile design with gingival architecture Adjunctive injectables like Botox/fillers as adjuncts for perioral harmony Final Takeaway Teeth may steal the spotlight, but the supporting gums and lips are what make a smile truly beautiful. Soft tissue aesthetics bridges the gap between oral health and facial harmony, helping dentists deliver results that are not just functional, but life-changing. Investing in these procedures can set a practice apart, enhance patient trust, and significantly increase treatment value. References Agarwal S, Sachdev SS, Mistry LN, Patel JJ, Patel NA, Shah T. Soft tissue management in implant dentistry: A comprehensive review. Cureus. 2025;17(2):e79557. SENAME Consensus Conference. Peri-implant soft tissue: SENAME Consensus Report. Clin Oral Implants Res. 2018;29(Suppl 15):7–10. Sourour ML, Tawfik OK, Hosny M, Fawzy El-Sayed KM. Evaluation of minimally invasive esthetic crown lengthening using an open flap versus flapless surgical approach: a randomized controlled clinical trial. J Esthet Restor Dent. 2024 Oct;36(10):1353-62. Thoma DS, Cosyn J, Fickl S, Jensen SS, Jung RE, Raghoebar GM, Rocchietta I, Roccuzzo M, Sanz M, Sanz-Sánchez I, Scarlat P, Schou S, Stefanini M, Strasding M, Bertl K; Working Group 2 of the 6th EAO Consensus Conference. Soft tissue management at implants: summary and consensus statements of Group 2. Clin Oral Implants Res. 2021;32 Suppl 21:108-12. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8596754/ Alammar A, Heshmeh O, Mounajjed R, Goodson M, Hamadah O. A comparison between modified and conventional surgical techniques for surgical lip repositioning in the management of the gummy smile. J Esthet Restor Dent. 2018 Nov;30(6):523-531. doi:10.1111/jerd.12433. PMID:30412347.

Social Media in Aesthetic Dentistry: Hype vs. Reality
Social media is no longer just a tool for connecting with friends; it is now a powerful driver of patient choices in healthcare. For aesthetic dentistry in particular, Instagram and Facebook have transformed how patients discover treatments, clinics, and eventually decide on procedures. For dentists, it provides an opportunity and a responsibility to harness these platforms and showcase expertise, build trust, and ethically educate patients. Why Social Media is Driving the Boom in Aesthetic Dentistry? Over the last decade, demand for smile makeovers has definitely surged, and social media is a huge driver. Patients don’t just want a service; they want to see proof, hear stories, and imagine themselves in the “after” photo. A single scroll through Instagram can inspire someone to book whitening, veneers, or even full-mouth rehabilitation. In fact, a 2024 study found that 29.4% of patients who pursued aesthetic dental treatments reported influence of social media content in their decision, especially visuals shared by clinics and dentists1. Trust vs. Misinformation Trust matters more than ever. Recent research showed that almost 62.5% of respondents preferred receiving dental health information via social media, and 36.7% said they trust only content from dentists or people they know2. On the other hand, misinformation is a growing challenge. A content analysis revealed that 86.8% of posts about oral health treatments were misleading3. This gap creates an opportunity for dental professionals to provide authentic, evidence-based information. What’s Trending: From Hashtags to High Demand? Most popular treatments: Teeth whitening consistently leads the pack, followed by veneers and orthodontic treatments, which are heavily driven by visual content. Engaged demographic: Women in their late 20s to mid-30s are often the most active audience for aesthetic dentistry content online. Instagram remains the leading platform, with Facebook following close behind. The ethics dilemma: Even dental students are not immune to influence. Studies show that exposure to social media can shape how future professionals view cosmetic treatments4. Beyond Posting: Educate, Engage, Convert Posting before-and-after photos is no longer enough. Clinics that stand out are those that educate and engage, not just advertise. Education wins: Studies show that educational posts (explaining treatment options, sharing preventive tips) consistently outperform purely promotional ones on engagement metrics. Show your process: Videos of procedures, behind-the-scenes stories, and Q&A sessions help humanize your practice and build trust. Know your audience: Tailor content for your most engaged demographic. Short-form video and interactive posts perform especially well. Social media isn’t just about likes; it’s a patient education channel that shapes treatment expectations. The Ethics Challenge: Influence vs. Integrity The rise of social platforms brings a unique challenge and makes one wonder how much influence is too much? Studies show that patients and even dental students are swayed by what they see online. For practitioners, this means balancing confidence in marketing with a commitment to accurate, responsible communication. Your post shouldn’t just inspire, it should also inform. Building authority in aesthetic dentistry is not about showing the perfect smile, but about showing the truth behind it. Key Takeaways for Dental Professionals Be visible, but stay credible. Patients are looking to you for trustworthy information. Prioritize education. Share authentic, fact-based content that addresses patient concerns. Leverage platforms strategically. Focus on Instagram and Facebook, where your most engaged demographics are. Mind the ethics. Avoid exaggeration; long-term credibility matters more than short-term clicks. References Freire Y, Gómez Sánchez M, Sánchez Ituarte J, Frías Senande M, Díaz-Flores García V, Suárez A. Social media impact on students’ decision-making regarding aesthetic dental treatments based on cross-sectional survey data. Sci Rep. 2024 Sep 16;14:21626. doi:10.1038/s41598-024-63341-9. Alhuzili G, Alghamdi A, Alhazmy R, Abdullah H, Sembawa S, Khayat W. The impact of social media posts concerning esthetic dentistry on self-esteem and satisfaction among adults in Saudi Arabia. Open Dent J. 2022 Mar 28;16:e187421062202141. Alfaraj A, Alshahrani FA, Albalawi M, AlQahtani N, Alhajji M, Alharbi AS, Ainoosah S, Al-Khalifa KS. Misinformation or education? A comparative analysis of Instagram posts related to full mouth rehabilitation. Front Dent Med. 2025 Jul 24;6:1585575. Freire Y, Gómez Sánchez M, Sánchez Ituarte J, Frías Senande M, Díaz-Flores García V, Suárez A. Social media impact on students' decision-making regarding aesthetic dental treatments based on cross-sectional survey data. Sci Rep. 2024;14(1):21626.

The Future of Dental Revenue: Subscription Models That Actually Work
For many dental practices, revenue feels unpredictable. Months swing up and down depending on seasonality, patient flow, or treatment acceptance. A subscription-based model offers a way to stabilize income, improve patient retention, and differentiate your practice. It is shifting from a “pay-per-visit” mindset to a membership approach, where patients pay a recurring fee for preventive and routine care. Why Subscription Models Work in Healthcare? Subscription or membership care isn’t new—it has been growing in medicine (concierge and direct primary care). Dental practices are now adopting this with in-house membership plans covering checkups, cleanings, diagnostics, and discounts on restorative work. Improved patient loyalty: A 2020 analysis of subscription models of direct primary care models predicted higher continuity and patient engagement by removing fee-for-service barriers and encouraging stronger physician–patient relationships1. Reduced cost barriers: In dentistry, studies show that patients without insurance delay preventive visits. Membership plans lower upfront financial uncertainty, which improves preventive utilization. Smoother revenue flow: Subscriptions generate a predictable monthly cash flow that protects practices from seasonal dips. What Should a Dental Subscription Plan Include? A subscription model may include - Core Preventive Care: Bi-annual exams, cleanings, X-rays. Discounts on Restorative/ Cosmetic Treatments: Typically 10–20% off. Family Packages: Encourage household enrollment to increase case acceptance. Tiered Options: Basic, Comprehensive, Senior plans so patients can pick based on needs. Patients appreciate predictability. Research shows that in-office membership plans often reduce cost confusion and are easier to understand than traditional insurance, which can increase willingness to enrol and engage. A 2024 article found that membership models simplify patient experience and aid higher engagement2. How to Implement in Your Practice? Here is a step-by-step guide to implement the structure for your dental practice - 1. Start Simple, Then Scale Don’t overcomplicate at launch. Begin with a single-tier preventive plan and only expand once uptake is stable. 2. Leverage Technology Use dental membership software or integrate with your practice management system. Automate billing, renewals, and reminders to reduce admin load. 3. Train Your Team Reception and treatment coordinators should confidently explain membership benefits. Patients often adopt when the value is framed in terms of saving on preventive care + predictable costs. 4. Promote Wisely Highlight “No Insurance? No Problem” messaging. Use chairside discussions, website banners, and recall emails. Target uninsured patients as data suggest that only 30% of women aged 15–49 and 33% of men aged 15–49 are covered by health insurance or a health scheme. It implies that approximately 70% of adults in this age group are uninsured, hence a big market for membership plans3. Measurable Benefits Revenue stability: Membership plans help streamline operations, reduce administrative burdens, and improve patient engagement, factors that contribute to long-term practice sustainability1. Higher treatment acceptance: Membership patients perceive discounts and commit more readily to larger treatment plans. Reduced cancellations: Patients who have prepaid are less likely to skip preventive visits. Final Takeaway Dental membership plans aren’t just a billing alternative; they are a strategy to cut no-shows, build loyalty, and secure predictable revenue. By keeping pricing transparent and care accessible, practices can strengthen trust while patients feel more in control of their oral health. For forward-looking clinics, adopting this model isn’t just about filling the schedule, it’s about future-proofing the practice. References Cole ES. Direct Primary Care: Applying Theory to Potential Changes in Delivery and Outcomes. J Am Board Fam Med. 2018;31(4):605–611. Comstock J. Dental membership plans facilitate better patient care. Dental Economics. 2024 Oct 16 [cited 2025 Aug 28] Sharma SK, Nambiar D, Sankar H, Joseph J, Surendran S, Benny G. Gender-specific inequalities in coverage of publicly funded health insurance schemes in southern states of India: evidence from National Family Health Surveys. BMC Public Health. 2023;23:2414.
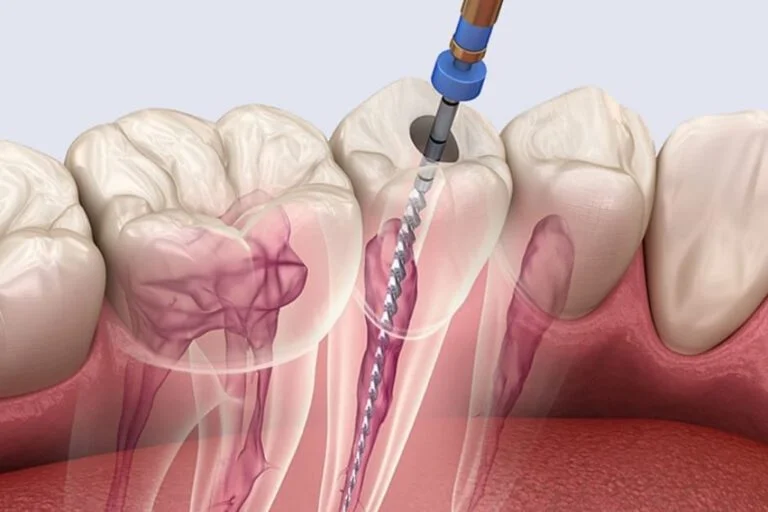
Tackling Calcified and Curved Canals
Let’s be real, tackling a stubborn calcified canal is not only a nuisance, it is a true litmus test for endodontic skills. To make it easier to handle the situation for the next case, here are a few subtle “tricks of the trade” that can help conquer these cases confidently and consistently. Why Calcified & Curved Canals Wreck More Cases Than You Think? Here is what one should know: up to 60% of root canal failures involve missed or inadequately treated canals, many of which are calcified or severely curved. These canals pose a triple threat: Hard to detect: Pulp chambers disappear like mirages on X-rays Hard to negotiate: Files bend, bind, or break mid-operation Hard to disinfect: Bacterial biofilms thrive in untouched canal recesses. If the clinician does not tackle these challenges head-on, they might be looking at a compromised prognosis with frustrated patients. 7 Clinical Hacks to Crack Calcified Canals Without Guesswork 1. Champagne Bubble Test The "Champagne Bubble Test" involves applying sodium hypochlorite (NaOCl) to the pulp chamber and observing for effervescence.1 Positive effervescence indicates the presence of organic tissue in hidden canals. This test is non-invasive and requires no additional equipment, making it a practical choice in routine endodontic procedures. 2. C-Pilot Files Combined with EDTA and Microultrasound Navigating calcified canals can be challenging. The combination of EDTA, C-Pilot files, and microultrasound can help by improving canal negotiation.2 The use of EDTA helps in chelating calcium ions, softening the calcified tissue, and, in addition, microultrasound aids in precise canal negotiation. 3. Reciprocating Motion in Curved Canals Reciprocating motion with clockwise 140 degrees and counterclockwise 45 degrees has been proposed to reduce the risk of file separation in curved canals.3 Utilizing reciprocating systems like WaveOne Gold can enhance safety and efficiency in curved canal preparation. 4. Pre-Bending Files for Canal Negotiation Pre-bending files is an effective yet overlooked trick in navigating calcified or curved canals. Endodontists with years of experience recommend this for the practicality in negotiating challenging canals. 5. Tapered Access Preparation for Improved Canal Entry Creating a tapered access cavity facilitates straight-line access to the canal system. Wider coronal prep is standard in endodontic access preparation, which helps reduce the file stress and improves canal negotiation.Focusing on the glide path improves file centring and minimises perforation risk.4 6. Use Warm NaOCl with Passive Ultrasonic Irrigation (PUI) Heat sodium hypochlorite to 40°C and activate with ultrasonic agitation (e.g. IrriSafe). Studies show that this method removed 65% more biofilm than syringe irrigation.5 7. Heat-Treated NiTi Files Traditional stainless steel files snap under stress in curved canals. Switch to heat-treated NiTi files like HyFlex EDM or ProTaper Gold that ‘remember’ their shape but stay flexible enough to navigate bends gracefully. Use a gentle, pecking motion with minimal force without rushing the glide path. Mastery and Mishap Extreme curvatures (>25°) demand respect and finesse. Here is a summary of how to stay in control: Always create a glide path with small hand files to reduce torsional stress on rotary instruments. Use a ‘crown-down’ approach, enlarging coronal thirds first to improve straight-line access. Opt for controlled memory NiTi files that adapt to canal curvature without forcing the shape. Avoid forcing files when resistance is felt. Retreat and reassess with irrigants or ultrasonic agitation. Be mindful of your working length at all times. Over-instrumentation risks ledging and perforation. Final Thoughts Managing calcified and curved canals is about strategy, not struggle. With the right tools, protocols, and insight, you can reduce failures and increase case predictability, all while preserving your confidence (and your rotary files). References Mirza AJ, Faruqi FA, Moosa R. Champagne bubble test: An authentic method to find hard-to-find canals during root canal therapy. Acta Sci Dent Sci. 2021;5(10):68-71. Chu T, Ni X, Zhu Y. EDTA combined with C-Pilot files and microultrasound for root canal calcification: dredging effect and safety analysis. Comput Math Methods Med. 2022;2022:1911448. You SY, Kim HC, Bae KS, Baek SH, Kum KY, Lee WC. Shaping ability of reciprocating motion in curved root canals: a comparative study with micro-computed tomography. J Endod. 2011 Sep;37(9):1296-300. Lup VM, Malvicini G, Gaeta C, Grandini S, Ciavoi G. Glide path in endodontics: A literature review of current knowledge. Dent J (Basel). 2024 Aug 14;12(8):257. Joy J, Mathias J, Sagir VM, Babu BP, Chirayath KJ, Hameed H. Bacterial biofilm removal using static and passive ultrasonic irrigation. J Int Oral Health. 2015 Jul;7(7):42–7.